I’ll never forget my patient Laura*, a 42-year-old wife and mom of two who, just weeks earlier, received a devastating diagnosis: metastatic pancreatic cancer. I met her and her family in the hospital after she was admitted for a second time because her disease had progressed and our palliative care team was brought in to deliver care and support.
Over the course of five months, we walked with her and her family as they navigated an emotional roller coaster of anger, denial, frustration, and finally, acceptance. We delivered care such as pain management, emotional support, and spiritual care that helped them explore their faith and spirituality in a supportive environment.
Laura’s symptoms were well managed, and she and her family felt more at ease and were able to focus on living life together. Without this type of support, they would likely be up against fragmented, uncoordinated care, struggle with shared decision-making, and experience caregiver stress and burnout.
As healthcare providers, we have the responsibility to educate patients and their families about the benefits of palliative care, clear up the misconceptions, and engage them in conversations about goals of care, advance care planning, and how they can experience a better quality of life.
What is Palliative Care?
The term palliative care is often misunderstood and many associate it with end-of-life care.
Palliative care is specialized care for people living with a chronic or serious illness. Patients receive support to experience relief from their pain and other symptoms, as well as to alleviate the stress of their illness.
The goal of palliative care is to improve the quality of life for patients and their families.
Palliative care helps patients and their caregivers develop goals of care and care plans for future challenges that may arise. They often receive education around advance care planning so if the patient is re-admitted to the hospital, or transitions to a lower-level setting such as a Skilled Nursing Facility (SNF) or primary care, information about their goals, values, and desires are in place.
Extending the Reach of Palliative Care for Serious Illness
There are 12M adults in the U.S. living with a serious illness who could benefit from palliative care.1 When we consider a generation of aging Baby Boomers, people living longer, and an increase in disease burden, these numbers are only expected to increase.
In the last decade, palliative care, has increasingly become a way to deliver the quality care and support patients need, reduce unnecessary utilization, and lower costs associated with serious illness.
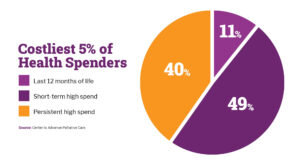
Most people with serious illnesses are neither dying nor hospitalized. In fact, only 11% are in their last year of life. Most are living at home, have longevity as their end goal, and need supportive care. Plus, people can have palliative care for years, and some can often “graduate” and transition back to their health plan’s care management program once they are at a steady state.
Of course, caring for those with serious illness is costly. This population makes up the 5% of patients driving over 50% of all health care spending.3 Spending that is a result of 911 calls, ED visits, hospitalizations, admissions into skilled nursing facilities (SNFs), and prescription medicines—which may be avoided with the right preventative care and support.
For those with serious illnesses, we must move from acute, episodic care toward preventative and holistic care if we want to drive better outcomes, improve quality of life, and reduce costs.
The Benefits of Home-Based Palliative Care
While palliative care in hospitals has increased, community and home-based palliative care has been largely underutilized—in part, due to a lack of access and awareness.
Given the shortage of doctors, nurses, and clinical staff, home-based palliative care solutions can fill a void and provide whole-person, coordinated care throughout the patient’s journey.
Palliative care in the home can offer a comprehensive, holistic approach to support patients and their families. This type of care helps to engage members in conversations for advance care planning, take into consideration their personal values and religious or spiritual beliefs, and if necessary, help with the transition to hospice.
Innovative home-based palliative care solutions that include a team of registered nurses and social workers add an additional layer of support for the patients and their providers.
The registered nurses focus on symptom management and care coordination. They have a comprehensive understanding of what patients have experienced thus far and what they can expect in the future. Members are provided with education, and compassionate care and support.
At the same time, social workers develop goals of care and facilitate advanced care planning. They uncover and address unmet social determinants of health (SDoH) through organizations in the community to alleviate any burden members and their families are facing, and provide resources, tools, and connections with local support groups for caregivers.
Improving Member Engagement and Access to Palliative Support in the Home
Member engagement and building trusted relationships are a key benefit to comprehensive palliative support in the home. This includes ensuring the appropriate cadence to deliver services, customize plans according to the days and times that work for members, engage with them in their preferred channels, and deliver culturally competent care and care in a members’ preferred language.
At CareCentrix, our home-based palliative support solution leverages predictive analytics that identify those who can benefit from supportive care earlier—helping to prevent unnecessary utilization of the ED and unnecessary hospitalizations.
Unlike other solutions, our palliative-trained team supports care coordination with members’ existing providers to ensure care continuity. Through our network and partnerships with local community-based hospice and palliative organizations, we can quickly and easily scale our program and ensure the same quality of care for all members regardless of their location.
Our palliative-trained care team can effectively close care gaps, address unmet needs, and prevent unnecessary, over-medicalized costs. When the time is right, we can help with the transition back to care management or to hospice. Our approach has a positive impact on member engagement, member satisfaction, and quality of life.
Learn more about our Home-Based Palliative Support solution and how we can help you improve quality of life, outcomes, and engagement for your members.
*Name has been changed.
EDRC 2026
Sources:
1)“Serious Illness: A High Priority for Accountable Care.” AJMC, July 2020. 2) “How do Health Expenditures vary across the population?” Peterson-KFF, 2021. 3) “Costliest 5% of Health Spenders.” Center to Advance Palliative Care.