The Challenge
Identify and close gaps in care that occur during transitions
The transition of care from hospital to home is a critical point in the patient journey, and failure to address gaps in care can lead to unnecessary hospital readmissions. It is estimated that 76% of Medicare Advantage hospital readmissions are avoidable.1
Successfully managing the transition of care for members requires the ability to assess risks, addressing clinical and non-clinical needs, with continuous engagement and monitoring to follow through on care plans and recovery. Many programs focus on 30 days post-discharge, but 50% of readmissions spend occurs after day 30.2 Medicare Star and HEDIS® measures are also increasingly focused on successful care transitions.

76% of Medicare Advantage hospital readmissions are avoidable.1
Program Results
- Impact on Star measures, including transitions of care2
- 22% reduction in hospital readmissions over 90-day program3
- 20% annual savings on readmissions spend3
- 95% medication reconciliations completed within 30 days3
- Positive impact on >60% of Star measures including transitions of care measures2

Our Approach
CareCentrix provides the analytics, member engagement, and care coordination to close gaps in care that may occur during transitions of care.
Through HomeFirst Analytics, each member receives a personalized risk assessment and care plan which anticipates the services required to close gaps in care. Our Care Transition Team, including physicians, nurses, social workers, and pharmacists, supports members’ transition home by:
- Reviewing the personalized care plans
- Addressing questions and education on follow-up care
- Monitoring the recovery progress
- Coordinating community support needs, such as meals, transportation, emotional or psychological support
Our Readmissions Management program supports Stars and HEDIS measures tied to the transitions of care measure, which includes medication reconciliation post-discharge, patient engagement, notification of inpatient admissions, and receipt of discharge information.
The CareCentrix Value
CareCentrix actively manages a seamless transition home and addresses gaps in care to reduce unnecessary hospital readmissions and costs for health plans.
Our Readmissions Management solution leverages HomeBridge®, our proprietary care coordination platform, which provides a single platform to document and access information offering complete transparency for providers and the care team. Our platform seamlessly integrates with health plans’ systems and includes automated data feeds, clinical notes, and authorizations to manage care effectively.
We provide a savings guarantee, and improve Stars and HEDIS performance for medication reconciliation, transitions of care, CAHPS, readmissions reductions.4
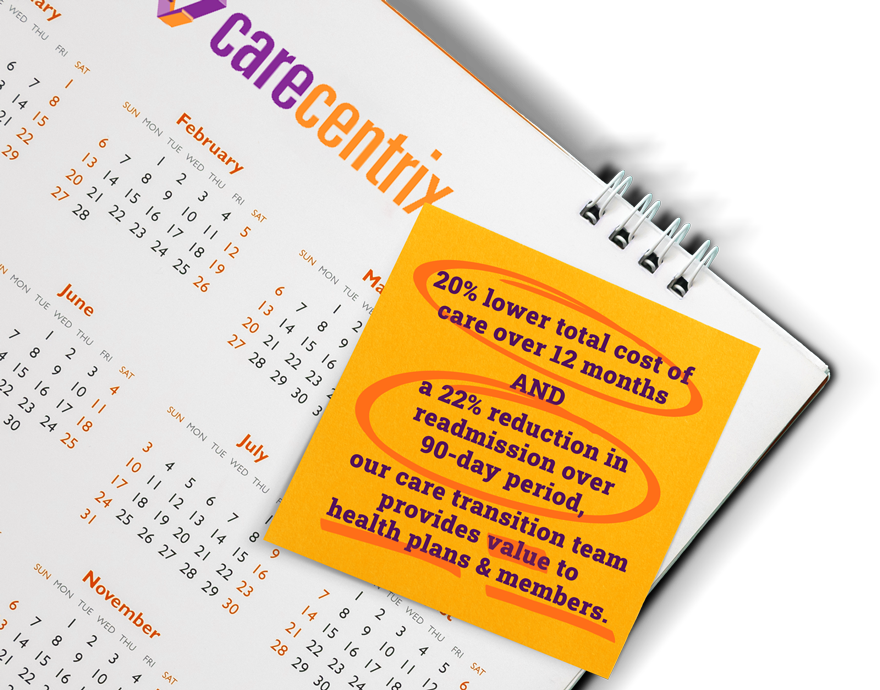
An independent study conducted by Avalere Health evaluated the impact of the CareCentrix post acute care program for Medicare Advantage populations and reported:
- Up to 20% savings on readmissions spend
- 22% reduction in unnecessary hospital readmission over 90-day period3