When we released our Health-at-Home-report in 2020, we were already seeing a trend that had been at play for quite some time: more care is being delivered in the home.
Among the results, we found that 91% of payors surveyed said advancements in telehealth or remote healthcare technology have encouraged their organizations to move care to the home. Plus, nearly two in three members said they prefer receiving care in their homes rather than going to a post-acute care facility.
97% of health plan executives say more care at home is better for insurers and members—CareCentrix Health at Home Report1
Although the shift to health at home continues to be on the upswing, a lot has changed in three years—innovative technology, new capabilities, and reimbursement changes, to name a few. Also, since the adoption of the Patient-Driven Groupings Model (PDGM), home health providers have increasingly moved to risk-based arrangements.
With an aging population of Baby Boomers, increased chronic disease burden and a rise in hospital spending, the shift to health at home shows no signs of slowing down. In fact, by 2025, up to $265 billion worth of services for Medicare beneficiaries could shift from traditional facilities to the home.2
5 Major Trends Impacting the Industry
As care increasingly moves to the home, there are several trends taking shape that will impact providers, payors, consumers, and the industry.
1. Staffing Shortages
Healthcare staffing shortages have plagued the industry for years and there’s no doubt they’ll persist. About one-third (31%) of nurses say they may leave their current direct patient care roles in the next year.3 And by 2030, the number of registered nurses needed will increase 28% from 2.8 million to 3.6 million.4
These shortages will continue to permeate into home health, making innovative solutions necessary to deliver quality services, improve health outcomes, and reduce costs.
2. Increased Technology in the Home
Telehealth, remote patient monitoring (RPM), and advances in data analytics have accelerated the shift to health at home. Over the next few years, expect to see technology play an even greater role in improving efficiency— allowing clinicians to focus more on delivering quality care to their patients.
By 2031, national health expenditures for home health are estimated to reach $250.6B5—CMS
3. Meeting the Needs at Home for Higher Acuity Members
Another emerging trend is an increased ability to care for higher acuity members at home. Although this type of care is still in its infancy, some payors already offer more complex services in the home, including infusion therapy and palliative support for members with serious illness.
Companies are also making investments to build out hospital-at-home and skilled nursing facility (SNF)-at-home solutions. These programs provide care for patients who would otherwise need to be in a hospital or post-acute care facility but may now have a choice to receive treatment and recover in the comfort of their own homes.
This ability to care for higher-acuity patients expands the population of those who can receive appropriate, more frequent, care in the home.
4. Reduction in Home Health Agency (HHA) Reimbursement
CMS continues to propose reductions in Medicare reimbursements to home health agencies, driving them to continually do more with less.
Therefore, over the next few years, payors will look to make changes to their home health strategy to ensure it’s sustainable. Starting with their provider networks, payors should contract with HHAs that can demonstrate their ability to deliver whole-person care in a timely manner and with proven results.
5. New Quality Measures for SDoH
Addressing the Social Determinants of Health (SdoH) has been a key area of focus for years. CMS has taken additional steps to measure how this is being addressed by Medicare Advantage (MA) plans by adding two new measures in 2024: the Social Need Screen and Intervention (SNS), and Social Connection Screening.
Advanced data analytics to identify unmet SDoH, strategies that drive engagement, and providers that deliver compassionate, culturally competent care are key components of whole-person care that can drive better outcomes.
Studies show that 80% of health outcomes are related to social needs such as health literacy, food, and financial insecurity.6
Home Health Strategies in 2024
For payors, these home health trends play a role in the shift to value-based care, emphasizing the need to reimburse providers based on their ability to deliver higher quality care to their members. But it won’t be easy. Whether it’s staffing challenges or incorporating new technology, payors must figure out how to make changes that incorporate these aspects into their future home health strategies.
As payors take steps to meet the growing demand for home health services, assessing their provider networks and understanding how to create a quality network that can meet the demands of home health will be key. Payors should focus on provider networks that can deliver on:
- quality care: demonstrate improved outcomes
- timeliness: ability to staff and deliver care in a timely manner
- access: using technology to extend the reach of care in the home
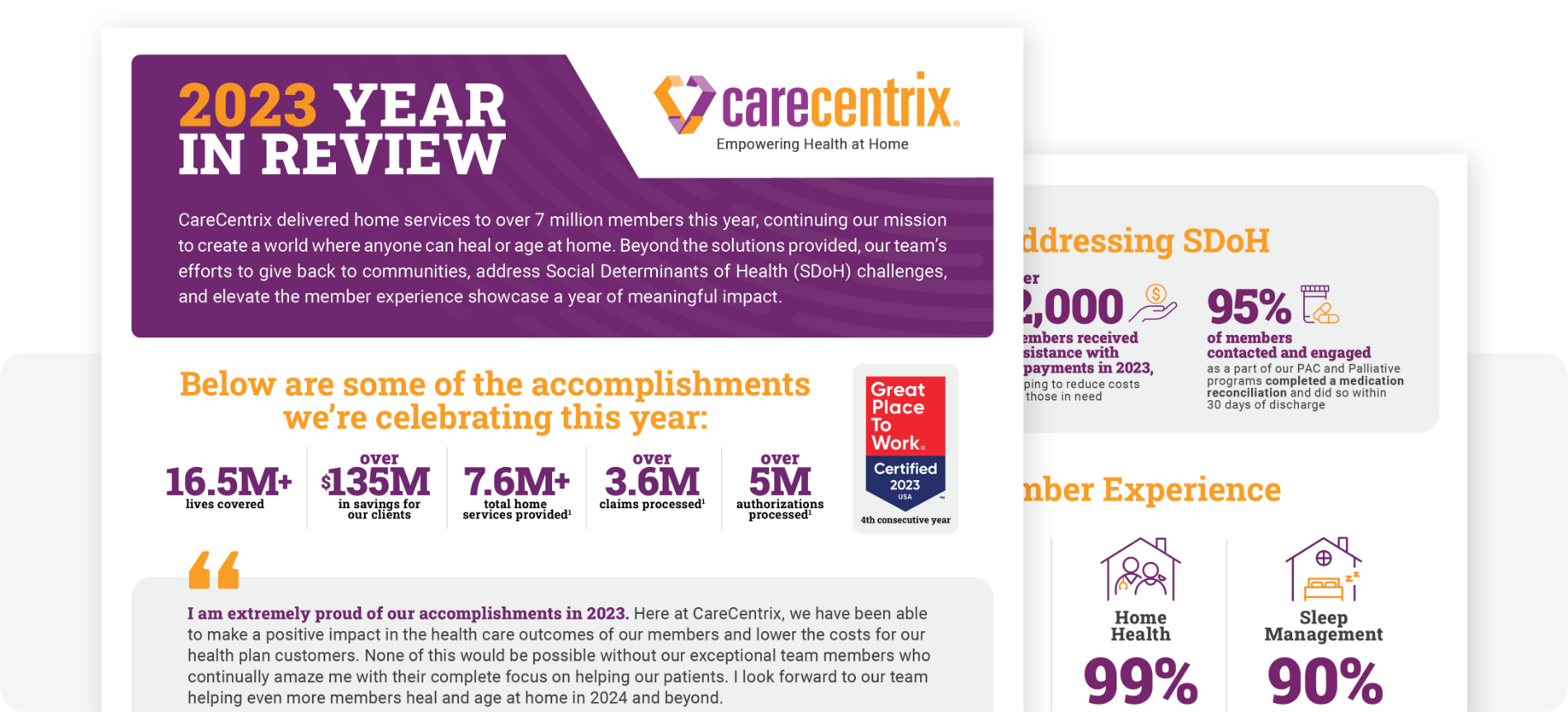
CareCentrix helps payors achieve better outcomes, and improve member satisfaction and Star Ratings. Through our high-quality home health provider networks, we have a 99% on-time start of care rate and 95% member satisfaction rate.7 Learn more about Home Health network management today.
Learn how we’re changing healthcare at home, read our latest blogs.
Sources:
- Health-at-Home 2020: The New Standard of Care Delivery. CareCentrix, 2020.
- “From facility to home: How healthcare could shift by 2025.” McKinsey and Company, 2022.
- “Nursing in 2023: How hospitals are confronting shortages.” McKinsey and Company, 2023.
- “The States with the Largest Nursing Shortages.” Registered Nursing.org, 2023
- “NHE Fact Sheet.” Centers for Medicare and Medicaid Services, 2023.
- “Screening for Social Determinants of Health: An Opportunity or Unreasonable Burden?” American Academy of Family Physicians, 2018.
- 2023 CareCentrix book of business performance data. Actual results will vary depending on program.
EDRC 2054