Why Culturally Competent Healthcare Is Vital To Whole-Person Care
Why Culturally Competent Healthcare Is Vital To Whole-Person Care


I’ve worked in healthcare for nearly two decades, and as a result, know a lot about the industry and what CareCentrix can bring to the table.
When my older sister was diagnosed with Interstitial Lung Disease, a term used to describe a large group of diseases that cause scarring of the lungs,1 I learned she would need a double lung transplant. I felt completely overwhelmed by the thought of what my sister would endure to have a chance at life.
I was thrust into a new role as her advocate, and had to get up to speed quickly on her diagnosis, the treatment plan, and the long journey that lay ahead. I also needed to learn about Medicare and what was covered under her plan.
My sister is currently in phase one of her journey. She is continually undergoing testing and has various provider appointments— many of which I accompany her to. I’ve been attuned to the care she is receiving and I’ve paid close attention to the interactions she has with her various providers, and their level of engagement, sensitivity, and empathy.
While every appointment has been positive, one, in particular, stands out.
Early on, my sister met with the hospital social worker and was asked to complete a comprehensive questionnaire about her childhood, family, medical history, and life experiences. When the social worker reviewed my sister’s responses, what I experienced was refreshing and gave me an immediate sense of comfort.
The social worker demonstrated an understanding of my sister’s history and where she is today. The appointment wasn’t transactional—like so many often are—and she wasn’t just checking off the boxes. Rather, she was invested in building a trusted relationship with my sister, delivering culturally-competent care, and showing compassion for her as an individual.
Although this path has been extremely difficult, I’m grateful that I can walk alongside my sister and advocate for her. While I’ve always known that the work we do at CareCentrix is valuable for patients and their families, this experience has made me even more passionate about our organization because I know what’s possible.
Whole-person care: Addressing barriers to care
When it comes to whole-person care, it’s more than simply addressing a specific symptom or chronic condition. It’s a holistic approach that takes into account all of the factors that promote health or disease.1
In fact, research shows that health-related behaviors, socioeconomic factors, and environmental factors are modifiable health factors responsible for up to 80% of health outcomes.2
The path to better health outcomes requires advanced analytics, engagement, and compassion, which starts with cultural competency.
Why is culturally competent care important?
While payors have made progress with leveraging analytics to predict gaps in care, and improving on ways to engage with members, a key element of whole-person care is compassion—driven by cultural competency.
Cultural competency is defined as: the ability of systems to provide care to patients with diverse values, beliefs, and behaviors, including the tailoring of health care delivery to meet patients’ social, cultural, and linguistic needs.3
Cultural competency enables trusted relationships with patients that directly impact care delivery. A recent survey found that 31% of physicians agree that their level of cultural competency affects their ability to provide the best possible care for their patients either somewhat or a lot.4
Delivering culturally-relevant care is also an important factor in reducing healthcare disparities, improving patient outcomes,5 and driving engagement.
An engagement strategy that incorporates cultural competency requires an understanding of individual differences, and identifying and overcoming language and cultural barriers.
How to deliver compassionate, culturally competent care
As U.S. diversity continues to grow at a rapid pace,6 culturally-competent care will be critical to reduce barriers, improve access, and promote health equity.
A whole-person model connects an individual’s unmet medical, emotional, and social needs, addresses their personal goals, and honors their personal beliefs. With a focus on cultural competency, care teams are better equipped to identify and address non-clinical needs in a way that builds trusted relationships and improves care.
Providers should be trained to:
- understand cultural values, traditions, beliefs, practices, and attitudes
- listen to patients’ health concerns
- demonstrate compassion
- communicate responsively and respectfully
A whole-person approach can close gaps in care, improve quality of life and health outcomes, reduce unnecessary readmissions, and decrease caregiver stress. But practicing compassionate, culturally-competent care, trusted relationships between providers and patients are built, patients receive higher-quality care, outcomes improve, and health equity can be achieved.
Want to learn more? Contact us today.
EDRC 1980
References
- National Center for Complementary and Integrative Health.
- National Academy of Medicine
- Health Research & Educational Trust
- Healthgrades
- BMC Nursing
- Brookings
Related Blog Posts
From Hospital to Home: The Unique Role of Nurse Liaisons
In celebration of National Nurses Month, we’re highlighting a couple…

How Can the Home Address High Costs of Chronic Disease?
Between the aging Baby Boomer generation and an increased disease…

Low Health Literacy is Costing Health Plans
90% of People Have Low Health Literacy–And It’s Costing Health…

How Whole-Person Care Can Lower Cost of Care for CVD
Cardiovascular Disease (CVD) is a key area of focus for…

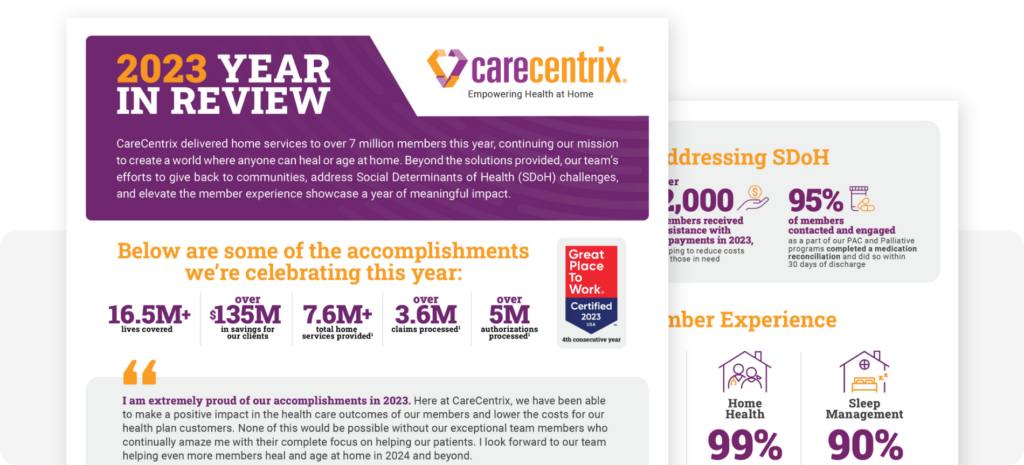
2023: Year in Review
CareCentrix delivered home services to over 7 million members this…
Defining Vulnerable Populations in Healthcare
Defining Vulnerable Populations in Healthcare As providers, health plans, and…

