Cardiovascular Disease (CVD) is a key area of focus for Medicare Advantage, Medicaid Managed Care Plans, and commercial payors. Nearly 50% of older adults in the U.S. have CVD, a group of disorders of the heart and blood vessels that can include coronary heart disease, stroke, and peripheral arterial disease. CVD is also the leading cause of death in the U.S., and the most expensive disease for payors to treat—costing $251 billion a year in direct medical costs.1
Although CVD is largely preventable, rising rates of diabetes, obesity and increases in the over 65-year-old population will continue to impact this growing trend. By 2035, the number of those with CVD is projected to increase to 131.2 million—representing 45% of the total U.S. population.2
Unfortunately, many people are not aware of their risks prior to a catastrophic event such as a heart attack, stroke, or even amputation. Treating CVD at more advanced stages leads to poor outcomes for members including hospitalizations and reduced quality of life, and higher spend for payors.
Once a person has CVD, whole-person care with a patient-centric approach remains a critical part of the health journey. Ensuring right care is in place and medication adherence, particularly during transitions of care such as a hospital stay can optimize health outcomes and even reduce the risk of mortality from CVD.
Cardiovascular Disease Risk Factors
Cardiovascular disease is considered a multifactorial disease due to modifiable and non-modifiable risk factors that may include:
- Hypertension
- Elevated low-density lipoprotein (LDL) cholesterol
- Diabetes
- Smoking and secondhand smoke exposure
- Obesity
- Unhealthy diet
- Physical inactivity
While rates among men are expected to increase at a greater rate until 2035, projections show women aren’t far behind since risk factors for CVD among this group are also rising.
Cardiovascular disease and its associated risk factors disproportionately affect many racial and ethnic groups and account for nearly 40% of the disparity in life expectancy, between black and white people.2
Health equity and the social determinants of health (SDoH) also contribute to risk. Lack of access to medical care, health literacy, food insecurity, social stressors, and economic stability can all impact an individual’s ability to get preventative care, understand and engage in their care, stick to healthy exercise habits and purchase healthy foods. In fact, the percentage of people with CVD who face food insecurity more than doubled over the last 20 years, one study found.3
Cardiovascular disease can be prevented or mitigated with interventions such as:
- A heart-healthy diet
- Regular exercise
- Smoking cessation
- Managing risks such as elevated blood pressure and cholesterol, and controlling diabetes
- Ensuring adherence to medications prescribed to prevent or treat CVD
- Regular health visits and screenings
- Stress reduction
- Addressing behavioral health
Transitions of Care: A Critical Time to Address Cardiovascular Disease
For members who have been hospitalized, the transition from hospital to home is a critical point in the patient journey. Common gaps are new medications, behavioral health, and affordability risks. These factors can lead to poor outcomes, readmissions, and high costs. Two ways to address these gaps include:
Primary Care Follow-up
Members should follow up with a physician or advanced practitioner within a week of hospital discharge to review new meds, follow up on pending tests and better understand their new condition. Sometimes, however, members may not have a PCP, or their physicians may not have available appointments.
Over 100 million people in the U.S—nearly one-third— don’t have a PCP4—National Association of Community Health Centers
Medication Reconciliation
Members may return home with questions about new CVD medications or have medications at home they are not sure if they should still take. They may worry about side effects and they may not trust the new treatment. Or, they may not be able to afford the medication or even be able to get to the local pharmacy if they don’t have reliable transportation.
Medication nonadherence affects between 40-50% of people with chronic diseases5—The Permanente Journal
How to Engage Members Who Have Cardiovascular Disease
Payors are increasingly looking to whole-person care approaches to prevent CVD, better manage member populations with CVD, and reduce costs.
Through predictive analytics, engagement, and care coordination, payors can educate members—and their caregivers—about their conditions, explore and address barriers, and close gaps in care.
For example, payors can identify members who have CVD and haven’t seen their physicians, had an LDL cholesterol test, or are not filling their CVD medications. These data points can enable targeted outreach to address barriers to care that may be at play. Payors can support benefit changes to improve adherence as a tool to engage and improve outcomes.
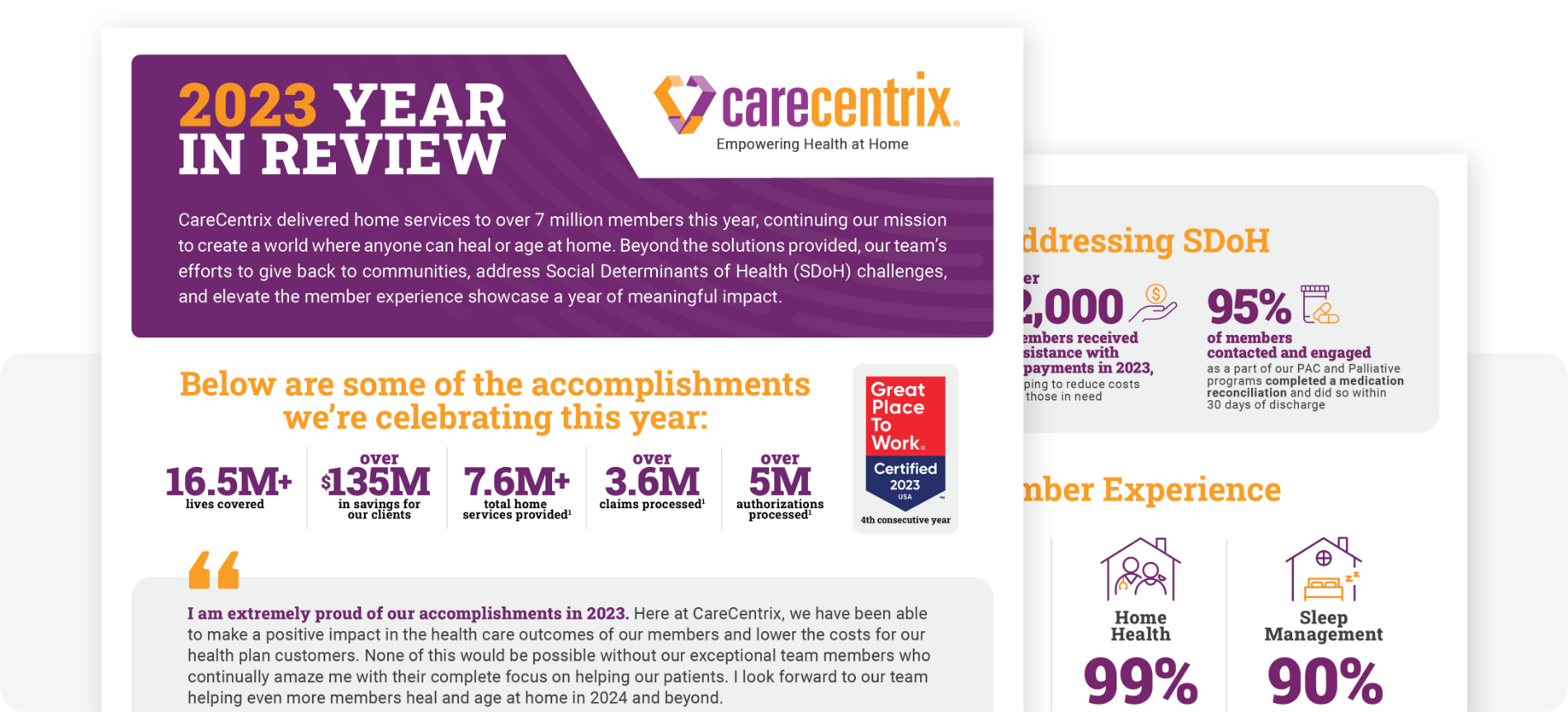
At CareCentrix, the 90-day Readmissions Management program leverages our HomeFirst Analytics to determine individual risk, providing direction for nurses to develop personalized care plans and close gaps in care. Our nurse coaches educate members about their conditions, conduct outreach to ensure timely follow-up care is in place, do careful medication reconciliation, and address unmet SDoH needs by encouraging members to work with community partnerships. Our program can support quality metrics to improve Star Ratings and HEDIS® measures, including Plan All-Cause Readmissions (PCR) and medication reconciliation post-discharge, to name a few.
Learn more about our Readmissions Management solution and how we can help you reduce unnecessary readmissions, the total cost of care, and help improve Star ratings.
[Footnotes]
Sources:
- “Heart Disease and Stroke Statistics – 2023 Update.” American Heart Association, 2023.
- Cardiovascular Disease: A Costly Burden for America.” American Heart Association, 2017.
- “Food Insecurity Among Individuals With Cardiovascular Disease and Cardiometabolic Risk Factors Across Race and Ethnicity in 1999-2018.” JAMA Network, 2022.
- “Closing the Primary Care Gap.” National Association of Community Health Centers, 2023.
- “The Unmet Challenge of Medication Nonadherence.” The Permanente Journal, 2018.
EDRC 2057