“Health happens in neighborhoods.”
This statement, from Dr. David Erickson, director of the Center for Community Development Investment at the Federal Reserve Bank of San Francisco, highlights the growing interest in social determinants of health at the local level. For Dr. Erickson, healthier neighborhoods are more prosperous and better educated, so the keys to better community health are better jobs and better schools.
The World Health Organization takes an understandably broader view. To the WHO, social determinants of health “are the conditions in which people are born, grow, live, work and age… [that are] responsible for health inequities – the unfair and avoidable differences in health status seen within and between countries.” The WHO focuses on national disparities in health outcomes.
What is common to both Dr. Erickson’s and the WHO’s definitions of social determinants of health is that they are too broad to help us understand what the real social determinants really are. Some clarification is in order.
Disengaging the weasel
Nobel prize-winning economist F. A. Hayek once described the word “social” as the “the great weasel word of our time.” A weasel word is one that sucks the meaning out of the word next to it, as a weasel sucks out the contents of an egg that it bites into. In other words, when we use the expression “social determinant”, we risk obscuring rather than defining what we mean by “determinant.”
To gently disengage the social weasel from the determinant egg, let us define what a “social determinant of health” actually is. For this purpose, the famous Whitehall studies of Sir Michael Marmot are instructive.
The social gradient
The Whitehall studies are a series of health-related surveys of British civil servants that began in 1967. The civil service is divided into a series of five employment grades, with the lowest grade represented by clerical workers and the highest grade represented by cabinet-level secretaries. Whitehall and colleagues discovered that there was a relationship between one’s civil service grade and mortality. The differences were not small: men in the lowest ranks had three times the mortality rate of men at the highest ranks. After controlling for confounding risk factors for chronic illness (obesity, smoking, low activity levels and others), the mortality differences persisted. Low social status appeared to be an independent risk factor for mortality.
The possible mechanism
Whitehall’s insight was that stress levels among civil servants correlated with their mortality. It is well-accepted in the medical world that stress and chronic illness are physiologically linked. The link appears to be the human immune system that has evolved to fight infection. It turns out that both acute and chronic stress trigger a cascade of reactions that result in chronic inflammation, helping to promote cardiovascular disease and diabetes, currently two of the major contributors to mortality. Whitehall’s hypothesis was that the stresses associated with having lower social status indirectly contributed to development of chronic disease, and hence mortality.
Stress and life
Social determinants of health, therefore, may be thought of as any factor in our lives that adds to our levels of chronic stress. These factors may be related to employment conditions. They may be related to social exclusion, or simply isolation. They may be related to adverse health habits that are common to an individual’s community, including smoking, excessive alcohol consumption, lack of physical activity and poor or inadequate diet. All these factors have been linked to stress-related chronic inflammation that shortens lives.
Tackling social isolation
The current medical model of health care has labored mightily to slow the progress of stress-related chronic illness, with little success. This failure may be related to the fact that there is not much modern medicine can do to alter the social determinants of health that give rise to chronic stress. Nevertheless, stress related to social exclusion is one area where our current health care system has a chance to do a great deal of good.
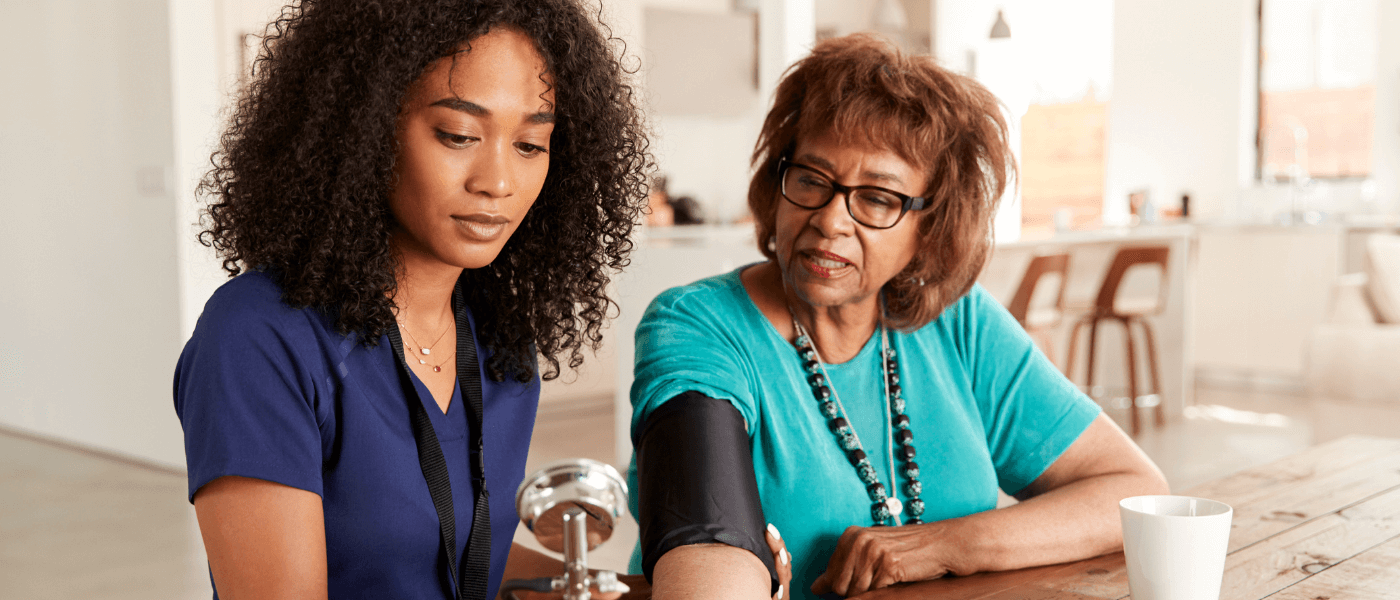
According to US Census Bureau, one in four Americans lives alone. This figure is likely to increase as couples continue to lose partners to age and disease. In response to the growing problem of isolation, the Centers for Medicare & Medicaid Services (CMS) has begun expanding home care services for Medicare recipients. CMS and the major private payers are beginning to realize that making the home the center of care may be the most cost-effective way to achieve good health outcomes. A distinct advantage of bringing health care home is that the human contact afforded by a home visit may help reduce the social isolation that the WHO and Dr. Erickson recognize as contributors to chronic disease and mortality.
Health may happen in neighborhoods, but it is essential to remember that neighborhoods include homes where many residents live alone. Helping those residents live healthier lives may be as simple as visiting them at home.