Each year, HLTH brings the entire healthcare industry together — connecting stakeholders to focus on pushing boundaries and moving the needle on better care for all. Over the four-day event, the CareCentrix team hosted many valuable conversations with attendees, networked with peers, customers, and partners, and listened to thought leaders in standing-room-only sessions.
With the recent announcement that Walgreens Boots Alliance would accelerate its full acquisition of CareCentrix, the event presented an opportunity for both companies to share more about the vision for a new consumer-centric healthcare delivery model that offers services at every stage of the care continuum. Walgreens will advance this mission through its newly formed U.S. Healthcare division, led by former CareCentrix CEO John Driscoll. The goal is to leverage a community-first model, supported by payor and provider-agnostic wraparound care, to improve member outcomes, better manage risk, and lower the total cost of care. During the event, John Driscoll participated in a panel to discuss what it means to take the right steps as a strategic leader in the evolving healthcare space. Walgreens executives Roz Brewer, Rina Shah, and Ramita Tandon each participated in sessions to share more about the company’s latest innovations and advancements in transforming the healthcare experience.
At HLTH 2022, one thing was clear: the conditions are right to advance this model in the coming years. We see three key areas of opportunity.
Turning on new channels for engagement
For many conference attendees, the central topic was engagement. The consensus is that the longstanding challenge of getting people to visit their doctors, adhere to medications, and manage their conditions is only becoming more daunting and disjointed. Patients are visiting their primary care physicians, the quarterbacks of their care, only 2.5 times per year – evidence that the traditional ways of connecting with a care team require the support of innovative solutions. There have been efforts to solve this problem with telehealth and digital health solutions, with varying degrees of success. The stark reality is that the market has become crowded, confusing, and in many respects, even more disjointed. Point solutions that focus on a specific disease or issue place the burden on patients – to manage different apps, portals, and devices and to share their health information across multiple platforms. While the intent is to create “personalized care journeys,” the patient experience is a tangled web of numerous “engagement silos.” Care becomes more uncoordinated, and the promise of personalization is just that – a promise. Partnerships focused on creating a connected ecosystem, and new channels must do better by focusing on eliminating barriers to care, improving access, addressing social determinants of health (SDoH), and health equity – with the ability to adapt to the changing behaviors of patients quickly.
Increasingly, more care will be delivered in the community via retail and at home, focusing on convenience. Community-oriented access to healthcare is the link to providing the right care at the right time with more personal service – keeping patients connected across the care continuum. The key is leveraging resources that patients already interact with in their day-to-day lives – whether that be at the pharmacy, doctor’s office, in-home, in the hospital, or virtually. This approach fosters long-term relationships, sustains behaviors, and removes barriers across the health journey, including those tied to SDoH and health equity.
Walgreens is uniquely positioned to tackle these challenges by leveraging a strong foundation of patient relationships and nearly 9,000 stores that serve as critical access points in communities across the U.S. The approach brings together their industry leading-companies, which are increasingly working together to keep patients connected to care at the community level.
Enabling a Whole-Person Approach
Increasing engagement and enabling a better relationship between the patient and care team is critical to provide whole-person care – another frequently discussed topic at HLTH.
Whole-person care encompasses coordinated care that addresses an individual’s physical, behavioral and social needs throughout everyday life to drive better outcomes – transforming episodic care into continuous care. Care teams face the challenge of meeting patients where they are with targeted, integrated programs that influence patient behavior, boost outcomes and control costs. While digital transformation, advanced analytics, AI, and point solutions are helping to address and support whole-person care, there are many signals that more is needed – particularly for individuals most at risk.
Once again, leveraging the community can be the solution. In a community-oriented care ecosystem, patients can access care teams that can identify social needs and activate resources to address them, often in the moments that matter. In some cases, having resources available in the community can help identify issues that even the patient may not have been aware of, like a patient who might be experiencing depression yet writes it off as just being stressed.
Value-based Care: Risk vs. Reward
As always, the key to making these models of engagement work rests in how we pay for it. And more than ever, value-based models were top of mind throughout the event.
Value-based care is essential for creating better engagement. It can enable a whole-person approach and incentivize the use of the home, typically the preferred site of care for patients and one that fosters better health outcomes. Value-based care models put the emphasis on prevention and early intervention, requiring some financial risk from payors and providers.
The innovations on display and the discussions at HLTH demonstrated that we’re in a better position to do this than ever. The convergence of better infrastructure and technology, streamlined care coordination, AI-driven clinical support, and value-based solutions can support efforts to reduce costs and expand access through digital, local community, and in-home channels. Implementing these can improve provider reach – opening up the ability to take the time to build relationships with patients that are more personal and trusted. The result yields the rewards of higher quality of care, better patient insights, and outcomes.
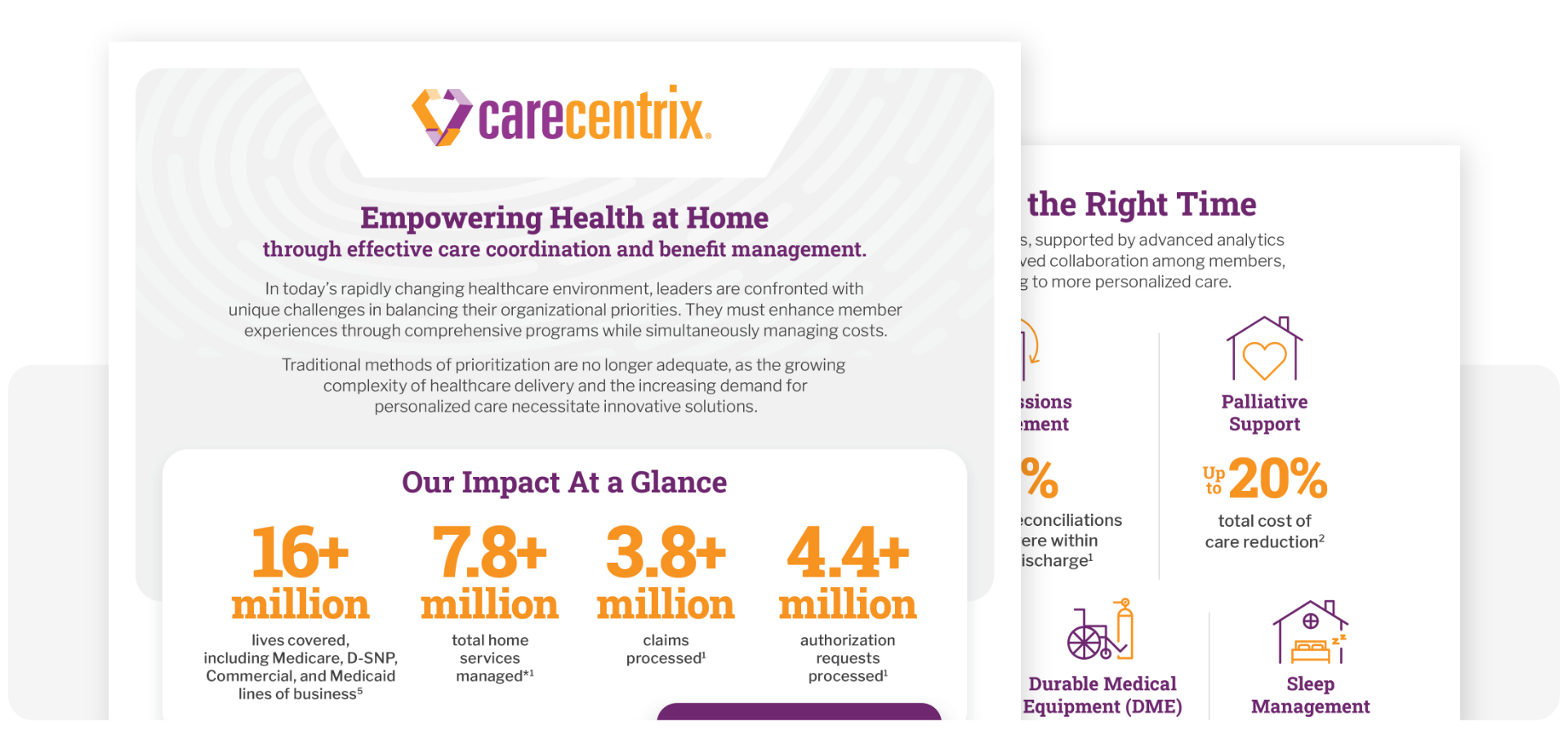
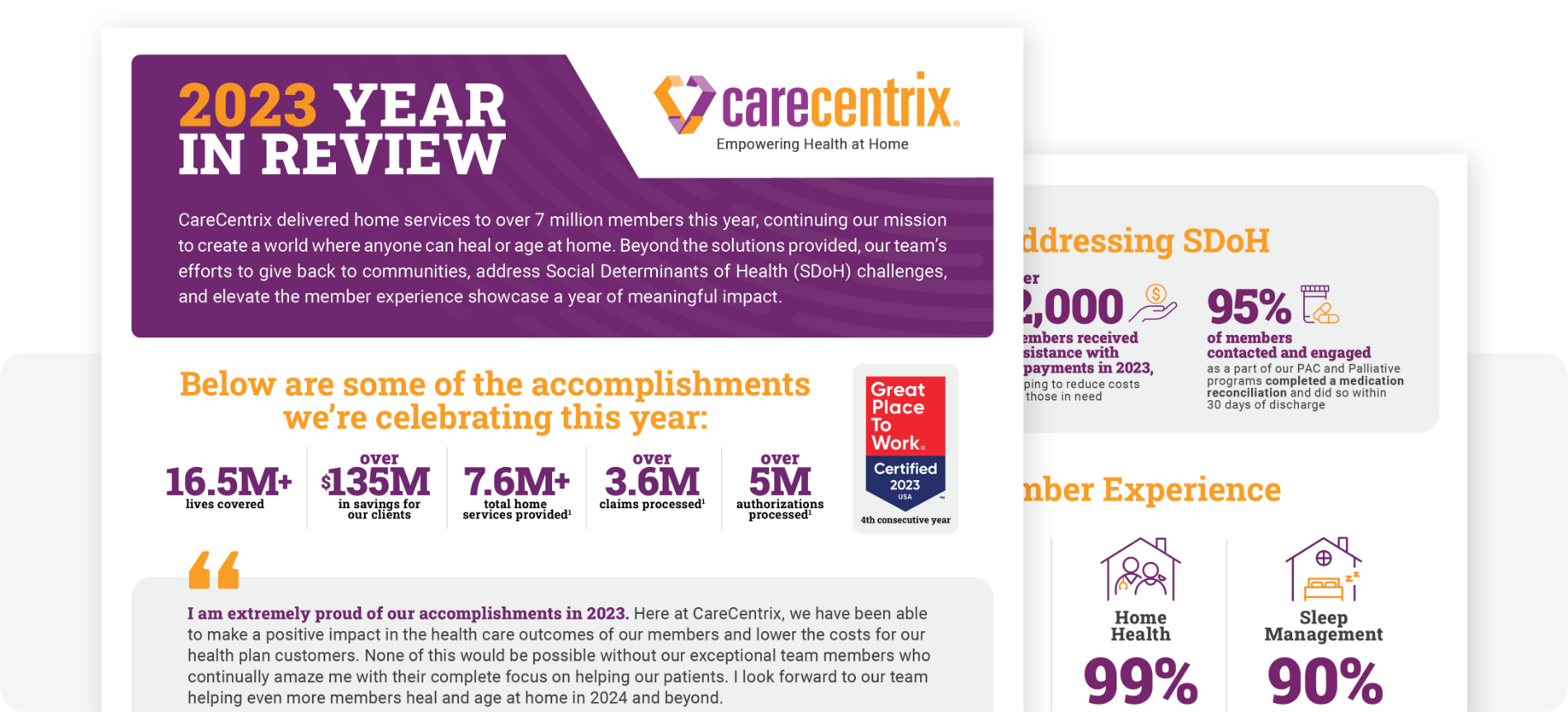
Here at CareCentrix, we offer payors value-based in-home benefit management solutions that improve outcomes, lower total cost of care, deliver member and provider satisfaction, enhance Star and HEDIS® measures, and guarantee savings. While there is much more to unpack, topline key takeaways for successful value-based care models include but are not limited to: stakeholder collaboration across the healthcare ecosystem, the willingness of commercial payors to embrace the models, coordination of care, patient-centered whole-person care and solutions, the ability to deliver “real” value, and a willingness to assume financial risk.
Overall, there are many opportunities to implement new patient-centered models to make progress on improving access, bringing care closer to where people are, and creating a better experience for the patient. There is no better time than now to work together to execute and make those opportunities a reality.