The history of surgery parallels the history of medicine in general. In the era prior to the development of anesthesia, most surgical procedures were conducted on battlefields and in workplaces. For minor procedures such as suturing wounds, the physician would often visit the patient’s home and perform the suturing at the kitchen table. With the growth in both knowledge and technology, surgery came to be performed exclusively in hospitals. At the 1970s, the trend reversed: increasing numbers of procedures began to be performed in non-hospital settings. Today, the majority of surgical procedures take place in out-patient centers, and even in physicians’ offices. This is generally referred to as “ambulatory surgery”, meaning non-emergent and planned in advance. The patient is not expected to be admitted to an acute care hospital following the procedure.
Where do patients go after their procedures?
Ambulatory surgery has proved to be enormously popular. According to the Centers for Disease Control (CDC), in 2010 over 48.3 million surgical procedures were performed in ambulatory surgical centers (ASCs). Whereas a substantial number of ASCs are located within hospitals, an ever-increasing percentage of the total number of procedures is occurring in free-standing ASCs. This trend is occurring because fewer and fewer patients require hospitalization following their procedures. According to the CDC, 95% of patients return to their customary residence (typically their home). A further 2% are admitted to “observation status”, in which the patient remains for a number of hours following a procedure and then returns home. Only 2% are admitted to an acute care hospital (the remaining 1% are discharged to recovery care facilities or emergency departments, among other locations).
Readmission
Unfortunately, these spectacular statistics do not tell the whole story. The 95% figure cited by the CDC fails to recognize that substantial numbers of ambulatory surgical patients need to be admitted to acute care hospitals due to complications that develop later or were not apparent at the time of surgery. A 2013 study suggested that readmission within 30 days of an ambulatory procedure was as much as 30 times greater than the rate published by the CDC. Hospital readmission is a major concern for the Centers for Medicare and Medicaid Services (CMS). Cuts in reimbursement rates and other penalties may be imposed on providers who fail to meet CMS guidelines. Therefore, physicians have been working hard to reduce readmission rates following ambulatory surgery.
Best practices – making a good thing even better
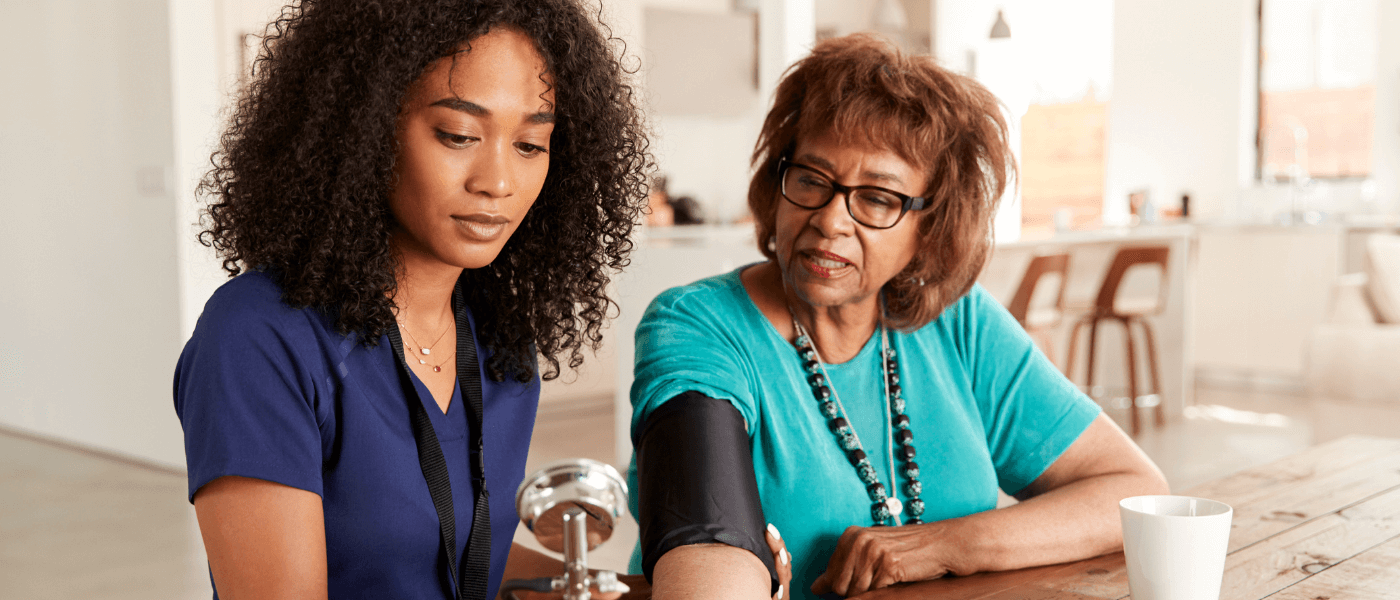
Organizations such as the Association of periOperative Registered Nurses (AORN) rigorously study surgical protocols and develop best practice guidelines aimed at reducing hospital readmissions. To develop these guidelines, AORN makes use of several tools. Valuable insights have been gleaned from the big data revolution, in which very large amounts of clinical data are mined and sifted to produce meaningful improvements in care. Many incipient complications may be forestalled by use of advanced remote patient monitors that allow real-time information to be transmitted to care providers. Finally, the increased availability of skilled home nurses can help prevent small complications from turning into hospital-level problems.
The future of ambulatory surgery
Ambulatory surgery blossomed in the pre-Internet era, without the benefit of big data or any of the types of Internet-based communications that are available today. There is every reason to believe that these technologies will accelerate the trend, while keeping complication rates low and reducing hospital readmissions. The question remains open as to the future of home-based surgical procedures. When that day arrives, we will have come full-circle to the era when the physician would suture wounds in the patient’s kitchen. Only this time, the doctor may bring a laser to correct the patient’s vision, or a portable biopsy device to remove suspicious moles.