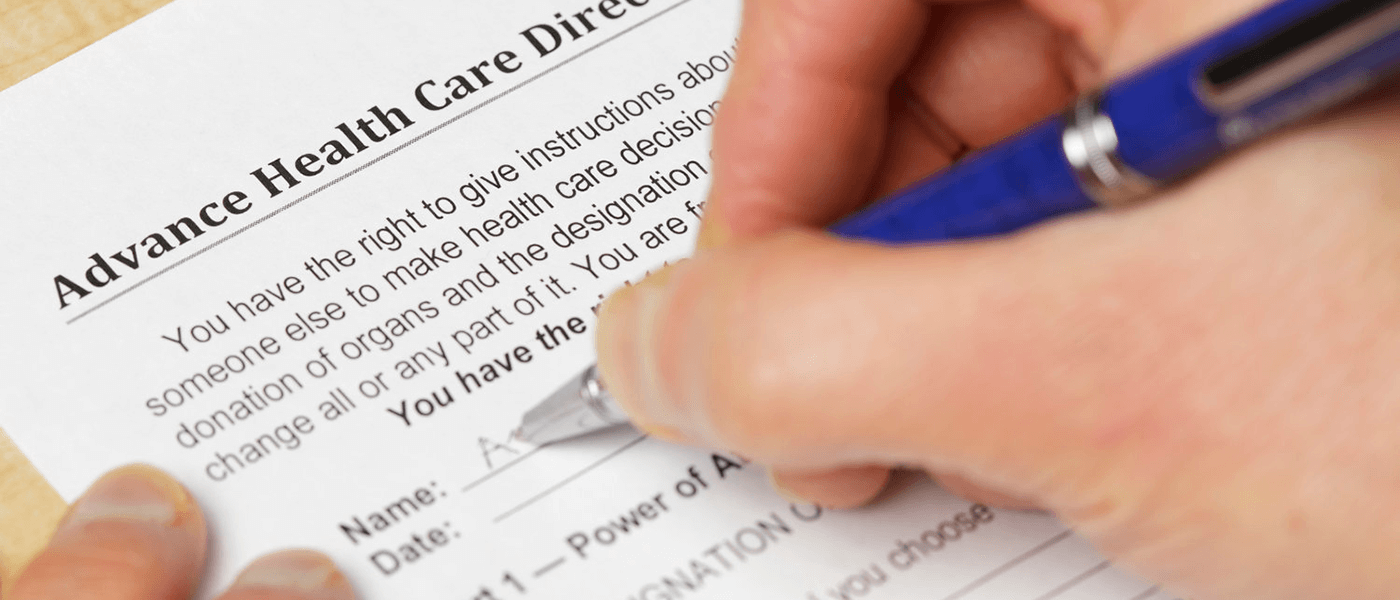
Completing advance directives (ADs) — legal documents that instruct physicians on how to carry out medical decisions – is one of the most important things that every adult, regardless of age or health status, should do. This is a person’s best way of ensuring that their wishes for end-of-life care will be carried out. ADs allow people to communicate with doctors, relatives, and friends when they are unable to do so during a medical crisis. This includes Durable Power of Attorney for Healthcare, a Living Will, and a form confirming the Physician Orders for Life-Sustaining Treatment.
End-of-life care plans and decisions are far from one-size-fits-all. Ideally, instructions expressing one’s care wishes should be part of everyone’s personal portfolio of documents. The goal is to ensure that the person’s wishes are respected while relieving stress, diminishing anxieties, and avoiding disputes among loved ones.
Despite the need and critical importance of Advance Directives in End-of-Life-Care, only 25 percent of Americans have recorded their end-of-life medical wishes in a legal document. This pervasive lack of advance care planning presents a problem because more than half of patients are unable to participate in end-of-life decisions when the time comes.
Whether or not an AD is in place, the goal is for providers to understand patients’ wishes on how they want to die, and whether treatment should be continued—and under which circumstances—or whether treatment should be ceased.
Meaningful Conversations: The First Step
When completing an advance directive, the individual should consider what is most important, asking such questions as “Who can make medical decisions with the physician if I am unable?” and “If your health situation worsens, what are your most important goals?”
It is often helpful to have these meaningful conversations with a healthcare professional who is trained and experienced with conducting these discussions. Sometimes, a physician is appropriate, but a growing number of a nurse or clinical social workers are now trained to facilitate these conversations.
Once a person has discussed their goals with family members to reach a shared understanding of their wishes, the next step is to make it official with an AD. While the process can sometimes be difficult, most people feel a sense of accomplishment — and greater peace of mind — after having the conversation and completing the AD process.
Legal Points to Consider
According to National Hospice and Palliative Care Organization, advance directives are legally valid throughout the United States. While a lawyer is not needed to fill out an AD, the individual’s AD becomes legally valid as soon as it is signed by the person in front of the required witnesses. Keep in mind that the laws governing ADs vary from state to state, so it is important to complete and sign ADs that comply with the state’s law. For instance, some states require the AD to be notarized, whereas others do not.
Given that one state’s advance directive does not always work in another state, the best solution is for patients to complete advance directives for the state or states in which they spend the most time.
To learn more about advance directives and specific state requirements, visit the National Hospice and Palliative Care Organization Advance Directive.