Critical Success Factors in Care Management for Building a Better Care Model for Seriously Ill Patients Living at Home
Critical Success Factors in Care Management for Building a Better Care Model for Seriously Ill Patients Living at Home


Download our latest white paper: Building a Better Model for Care at Home.
Turn-Key Health, a CareCentrix company, has reimagined the home as a destination of care for seriously ill patients. In our latest white paper, “Building a Better Model for Care at Home,” we demonstrate how home-based palliative care (HBPC) for individuals with a serious or advanced illness successfully aligns treatment decisions with personal goals, preferences and values; enables payors to reduce emergency department visits, hospitalizations and 30-day readmissions; addresses clinical and non-clinical issues, such as social determinants of health (SDoH); and provides an opportunity to enhance member and caregiver engagement and care coordination.
HBPC for the nation’s most vulnerable has never been more important as we head into 2021.
Promising Opportunity
Today’s elderly population is aging in a different way than they have in the past, as people live longer, stay active and have more options that enable them to remain in the home. Nearly 90% of seniors want to age in place and 72% of patients surveyed prefer home recovery: home is a comfortable, familiar environment where individuals can set their own schedules for food and sleep, enjoy less noise, less anxiety, better nutrition and better access to their support network and transportation.
One of the key goals is to make sure the information that’s collected during those home-based visits is also looked at longitudinally to identify and drive appropriate interventions when there is a change or advanced need in the home. Nurses conduct robust conversations with the patients — really getting to know them – and pick up on cues that would otherwise be lost. Our objective is to make sure this information is fed back through the system.
Optimizing Care in the Home
HBPC supports a structured approach to care for individuals and caregivers who need assistance with both clinical and non-clinical issues, providing an added layer for support services in the home. What is critical for these members is a timely response to non-medical issues, many of which are related to social determinants of health (SDoH), such as food inadequacies, access to reliable transportation and housing insufficiencies, as well as loneliness and isolation. Specially trained home-based palliative care teams identify and fill care gaps with appropriate resources for optimal care management.
Our innovative home-based care model, Palliative Illness Management™ (PIM), is a high-touch, program that blends the expertise of a clinical care team and methodology that is purpose built to support seriously ill patients in the home. This unique approach focuses on member and caregiver engagement, including ways to motivate patients and caregivers so that they are fully engaged in and motivated to choose and implement a plan of care and treatment that optimizes their quality of life.
As the cornerstone for building a better model for care at home for seriously ill patients, PIM can be scaled across broad and diverse geographic regions, spanning urban and rural communities.
When there are medical or ancillary needs, the clinician team contacts the treating physician and, for non-clinical issues, the team directly coordinates services. This facilitates effective collaboration between the palliative care team and the broader medical home and care management teams to extend the reach of physician practices.
Related Blog Posts
Family Caregivers: How Palliative Care Can Help
Facing a serious illness is overwhelming for patients, their family…

Moving Palliative Care from the Hospital to Home
Payors are constantly looking for ways to enhance the member…

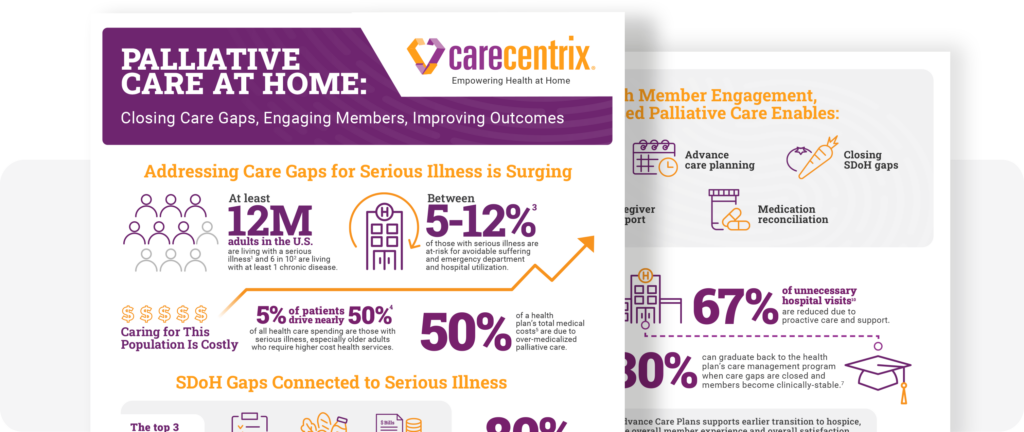
Palliative Care at Home: Closing Gaps, Engaging Members
Supporting members with serious illness can become costly. The need…
What is Home-Based Palliative Care?
I’ll never forget my patient Laura*, a 42-year-old wife and…

The Future of Serious Illness Care: 3 Ways to Improve Your Strategy
With serious illness care being a highly uncoordinated part of…
Paving the Way for Culturally Inclusive Palliative Care Services
Despite the benefits of palliative care, cultural differences often create…
